Introduction to Anemia
Anemia is not being tired. It is the body that must fight to get enough oxygen to operate. Essentially, Anemia occurs when our blood lacks sufficient healthy red blood cells or haemoglobin. The component of those cells that transports oxygen. Without oxygen, our organs cannot function properly. Therefore, individuals who have Anemia tend to feel weak and lightheaded after light activities.
Why is this being discussed particularly in India? Because Anemia is a rising public health problem here. The latest national statistics indicate that over half of Indian women between 15 and 49 years are anaemic. In children below five, the figure is even higher. The better news? Anemia is preventable and curable.
What Is Anemia?
Our body runs on oxygen. Every cell, from our brain to our muscles, needs it constantly. Red blood cells are the delivery guys. They carry oxygen from the lungs and drop it off where it's needed. The key to this delivery system is a protein called haemoglobin, which binds to oxygen inside those cells.
When someone suffers from Anemia, there are either not enough red blood cells or they don't carry enough haemoglobin. That means the oxygen supply is cut short. The body has to work harder to do basic things. So we feel tired, short of breath, or foggy-headed even after small efforts.
Anemia isn't a disease by itself. It's usually a signal that something else is wrong.
Doctors check the severity of Anemia based on haemoglobin levels in the blood:
- Mild Anemia usually doesn't show many symptoms.
- Moderate Anemia can cause tiredness, light-headedness, and pale skin.
- Severe Anemia can affect your heart and brain. In extreme cases, it becomes life-threatening.
What makes Anemia tricky is that it often goes unnoticed. People assume they're just overworked, not eating well, or stressed. But when ignored, even mild Anemia can snowball into serious health problems.

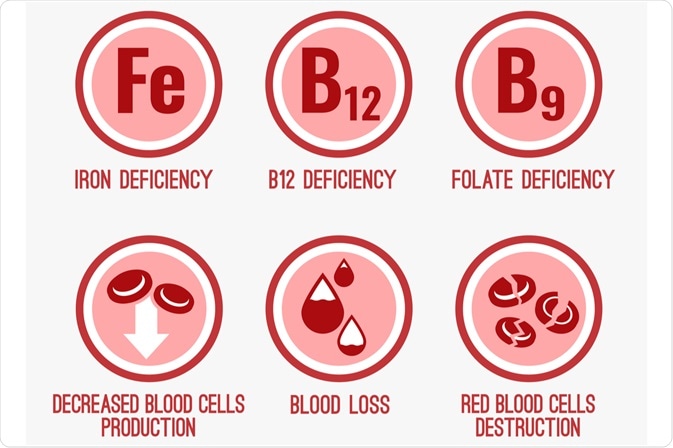
Causes of Anemia
Anemia doesn't come from just one thing. It's the result of an imbalance. Either our body is losing too many red blood cells, not making enough, or destroying them faster than it should. Here's how that can happen:
-
Blood Loss
This is one of the most common causes, especially in women. Heavy periods, childbirth, injuries, or internal bleeding (like from stomach ulcers or piles) slowly drain the body's iron stores. Over time, even small daily losses can lead to Anemia. -
Poor Nutrition
Our body needs iron, vitamin B12, and folate to make red blood cells. If our diet lacks these due to poverty, poor food choices, or restricted diets, then the body starts to produce fewer or weaker red cells. This is especially common in children, teens, and pregnant women who need more nutrients. -
Chronic Diseases
Conditions like kidney disease, cancer, HIV/AIDS, rheumatoid arthritis, or tuberculosis interfere with red blood cell production. In these cases, Anemia is part of a bigger issue; it's called Anemia of chronic disease. -
Genetic Disorders
Some people inherit conditions that affect how their blood works. Sickle cell Anemia changes the shape of red blood cells. Thalassemia affects haemoglobin production. These are lifelong conditions and more common in certain communities, including some tribal populations in India. -
Infections
Parasitic infections like hookworm and malaria are still widespread in many parts of India. These parasites feed on blood or damage red blood cells directly. Repeated infections can lead to chronic Anemia, especially in children living in poor sanitary conditions.
Symptoms of Anemia
Anemia doesn't always hit suddenly. It often builds up quietly, with everyday signs that are easy to ignore. But these symptoms are your body's way of saying it's not getting enough oxygen. Recognizing them early can help prevent complications and improve your quality of life.
- Fatigue and weakness: You may feel drained even after rest. Physical strength drops, making simple tasks feel exhausting.
- Pale or yellowish skin: A noticeable paleness, especially on the face, lips, or inside eyelids, is common. Some types of Anemia also cause a yellow tint to the skin.
- Shortness of breath: Even mild effort like climbing stairs can leave you breathless. This happens because your body lacks oxygen-carrying red blood cells.
- Rapid or irregular heartbeat: Your heart may beat faster or unevenly to make up for low oxygen levels. Chest pain can appear in more severe cases.
- Headaches and dizziness: Poor oxygen supply to the brain often causes light-headedness or persistent headaches.
- Cold hands and feet: Poor circulation due to Anemia can leave your extremities feeling chilly, even in warm weather.
- Unusual cravings (pica): Craving non-food items like ice, chalk, or dirt may signal iron deficiency Anemia.
If you notice these symptoms together, don't ignore them. A simple blood test can confirm the diagnosis and guide the right treatment.
Types of Anemia
- Iron Deficiency Anemia: Most common. Caused by poor iron intake or blood loss. Symptoms include fatigue, brittle nails, and cravings like ice-eating (pica).
- Vitamin-deficiency Anemia: From low vitamin B12 or folate. Leads to weakness and neuropathy-like numbness or tingling.
- Aplastic Anemia: Rare but severe. The bone marrow stops making enough cells. Leads to frequent infections and bleeding.
- Haemolytic Anemia: Red blood cells are destroyed faster than they're made. Causes jaundice and an enlarged spleen.
- Sickle Cell Anemia: An inherited condition that causes sickle-shaped red blood cells. Painful blockages and chronic Anemia are seen in tribal populations.
- Thalassemia: An inherited defect in haemoglobin production that causes microcytic Anemia and often needs lifelong transfusions.
- Anemia of Chronic Disease: Inflammation from chronic illness reduces red cell production.
- Pernicious Anemia: Autoimmune attack prevents absorption of B12, leading to similar symptoms to B12 deficiency.
Diagnosis and Tests
- CBC checks red blood cell count and haemoglobin.
- B12 and folate levels identify a specific deficiency.
- Reticulocyte count determines new cell production.
- A peripheral smear examines blood under a microscope.
- Bone marrow biopsy is rare. Used for aplastic or unexplained cases.
- Other tests, like endoscopy or colonoscopy, are used for bleeding. Kidney function tests for chronic disease.
Treatment and Remedies for Anemia
There's no one-size-fits-all treatment for Anemia. That's because the best remedy depends on what is causing it. Once a doctor figures out whether the problem is a lack of iron, a chronic disease, or a genetic condition, treatment can begin.
A. Medical Treatments
- Iron Supplements: For iron deficiency Anemia, doctors usually prescribe oral iron tablets. They're taken daily for a few months. In cases where the tablets don't work. Also, when someone can't tolerate the side effects like nausea or constipation, intravenous (IV) iron may be used.
- Vitamin B12 and Folic Acid: If tests show a lack of vitamin B12, patients may need injections once a week for several weeks. After that, maintenance doses can be taken as tablets. For folate deficiency, oral folic acid pills are usually enough.
- Blood Transfusions: In moderate to severe cases, especially during pregnancy or after serious blood loss, blood transfusions can raise haemoglobin levels quickly. These are done in hospitals and closely monitored.
- Erythropoietin: For people with kidney disease or cancer, doctors sometimes use a hormone called erythropoietin. It stimulates the bone marrow to make more red blood cells.
- Chelation Therapy: For conditions like thalassemia, patients may receive frequent blood transfusions. This causes iron overload in the body. To manage it, doctors prescribe chelation therapy. A special medicine that removes excess iron from the blood.
- Bone Marrow Transplant: In aplastic Anemia, where the bone marrow stops producing cells, a bone marrow transplant may be the only long-term solution. It's a major procedure and not suitable for everyone.
B. Natural and Home Remedies (Supportive Only)
These remedies can't replace medical treatment, but they support recovery and help prevent Anemia from coming back.
-
Iron-Rich Foods: Eating the right foods is key. Include:
- Dark leafy greens (like spinach and methi)
- Lentils, chickpeas, and beans
- Red meat, liver, and eggs
- Whole grains
- Jaggery (especially in rural diets)
-
Vitamin C Boosters: Vitamin C helps the body absorb iron better. Add:
- Citrus fruits (oranges, lemons)
- Amla (Indian gooseberry)
- Tomatoes and bell peppers
- Avoid Tea or Coffee with Meals: Tea and coffee contain compounds called tannins that block iron absorption. Try to avoid them at least an hour before or after iron-rich meals.
- Cook in Iron Vessels: It may sound old-fashioned, but cooking in an iron kadai or pans can actually increase the iron content of your food. Especially curries and acidic dishes like tomato-based meals.
- Regular Deworming: Worm infections, especially hookworms, can drain iron from the body. Regular deworming is essential. Especially for school-age children in rural areas. The government often provides free deworming tablets through schools and Anganwadi centres.
Fatality and Long-Term Impact
Untreated severe Anemia increases the risk of heart failure and fatal outcomes. It slows child growth and hampers cognitive development. For pregnant women, it raises the chances of low birth weight and preterm births. Chronic oxygen deficit overworks the heart and exacerbates other illnesses.
Anemia in India: Public Health Concern
India suffers from one of the highest Anemia rates globally:
- 57% of women aged 15-49 are anaemic (up from 53% in NFHS‑4)
- 67.1% of children under 5 are anaemic (up from ~59%)
- 25% of men aged 15-49 also have Anemia
Worryingly, mild and moderate cases are rising. This is especially acute in rural, tribal, and economically disadvantaged areas, where Anemia overlaps with malnutrition and weak maternal health services.

Government Schemes and Support for Anemia in India
India has some of the highest Anemia rates in the world. To tackle this, the government has launched several programs over the years. These schemes focus on prevention, early detection, and treatment.
A. Key Schemes Targeting Anemia
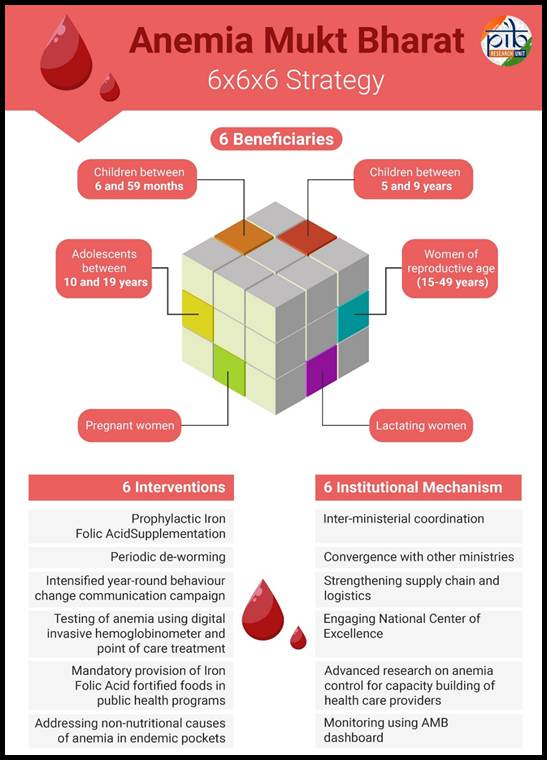
-
Anemia Mukt Bharat (AMB): Launched in 2018, AMB is one of India's biggest Anemia control efforts. It uses a 6×6×6 strategy:
- 6 Target Groups: children (6 - 59 months), adolescents (10 - 19 years), women of reproductive age, pregnant women, lactating mothers, and men.
- 6 Interventions: Iron and folic acid (IFA) supplementation, Deworming, Behaviour change communication, Testing and treatment at health facilities, Iron-fortified foods, Delayed cord clamping after delivery
- 6 Institutional Mechanisms: involvement of schools, Anganwadi centres, PHCs, and health workers for better implementation.
- POSHAN Abhiyaan: This flagship mission, launched in 2018, focuses on nutrition improvement. It targets pregnant women, lactating mothers, and children under six. It links Anemia control with better maternal and child health.
- Weekly Iron and Folic Acid Supplementation (WIFS): WIFS targets school-going adolescents (boys and girls aged 10-19 years) by providing a weekly IFA tablet and twice-yearly deworming. Delivered through schools and Anganwadis, this program plays a key role in prevention.
- National Health Mission (NHM): NHM funds many Anemia-related services like testing, treatment, and counselling. Especially in rural and underserved areas. It also supports ASHA and ANM workers in follow-up care.
- Janani Suraksha Yojana (JSY): This scheme promotes institutional deliveries with financial incentives. It also ensures that pregnant women receive proper check-ups, IFA tablets, and counselling to prevent Anemia during pregnancy.
- Rashtriya Bal Swasthya Karyakram (RBSK): RBSK screens children up to 18 years for 30 health conditions, including Anemia. Children found anaemic are referred for treatment through public health systems.
- PM POSHAN (formerly Mid-Day Meal Scheme): This provides iron-fortified meals to schoolchildren. The goal is to improve nutrition and learning outcomes while tackling hidden hunger, including iron deficiency.
B. Government Distribution Channels
Here's how these programs reach people:
- Schools and Anganwadi centres: Children and adolescents receive IFA tablets, hot cooked meals, and deworming tablets.
- Village Health and Nutrition Days (VHNDs): These monthly events offer testing, counselling, and supplement distribution in rural areas.
- Primary Health Centres (PHCs) and Community Health Centres (CHCs): Provide haemoglobin testing, prescriptions, and follow-up.
- Mobile Health Units: Used in hard-to-reach tribal and remote areas.
- IEC Campaigns: Posters, community meetings, and local radio promote awareness about Anemia and nutrition.
These schemes are interconnected. For example, a schoolgirl might receive IFA tablets through WIFS, eat iron-fortified rice via PM POSHAN, and get screened for Anemia through RBSK all at the same school.

Recent Initiatives and Data
India's Ministry of Health reports:
- 15.4 crore children and adolescents received IFA in Q2 FY 2024‑25
- Digital tracking using the Anemia Tracker App.
- Increased funding under POSHAN 2.0.
- Adolescent focus via the SABLA scheme.
- Integration into Ayushman Bharat Health & Wellness Centres.
Despite pandemic disruptions, IFA distribution rose notably from NFHS‑4 to NFHS‑5.
Major Steps in Bihar, Jharkhand & Gujarat
Gujarat
- Dr. Yazdi Maneksha Italia, leading Gujarat's sickle-cell control program since 2006, significantly improved tribal healthcare outcomes. His efforts earned him awards like Padma Shri (2024), PM's Award for Excellence (2011), and Chief Minister's Award (2023).
- In May 2025, the government approved Gujarat's first Centre of Competence for sickle-cell Anemia in Surat under the National Sickle Cell Anemia Elimination Mission 2047. This hub will provide specialized care, labs, training, cultural outreach in tribal dialects, and ICU support.
- Gujarat is also launching a tribal genome mapping project across 17 districts to study genetic predispositions, including Anemia and blood disorders.
Bihar & Jharkhand
- Frontline Worker Training (Test, Treat & Talk Approach) through Piramal Foundation's partnership. In early 2024, the government trained ANMs and health staff in hemoglobin testing, intervention counseling, and IFA adherence strategies. Compliance was low: only ~18% of mothers consumed IFA for 100+ days (NFHS‑5, 2019‑21).
- Bal Kuposhan Mukta Bihar (BKMB) is a state-run campaign (since 2014) under ICDS platforms focusing on behaviour change, capacity building, community participation, and nutritional awareness to tackle child malnutrition and Anemia.
- District-Level Recognition in 2024–25, Saran district achieved third place in Bihar's "Anemia‑free ranking" with a 93.2% score based on HMIS data tracking IFA coverage and outcomes.
- In Jharkhand, especially among tribal communities, mobile health units support sickle-cell screening, often integrated into PM-JANMAN development programs. For instance, the Gumla district launched a multi-pronged strategy including sickle-cell Anemia screening, nutrition kits, health camps, and Anganwadi outreach under PM‑JANMAN.
Major News Highlights and Awards for Anemia
News Highlights
- CSIR, via its CCMB lab, is developing an affordable sickle‑cell test kit priced under ₹100, expected within six months. An innovation that promises accessible diagnosis in rural and tribal populations.
- The ICMR has mandated rapid testing kits for sickle cell Anemia alongside Hepatitis‑B and syphilis—to be available at rural health centres, Ayushman Arogya Mandirs, Sub-Centres and PHCs across India, expanding early detection and preventive access in underserved areas.
- Daga Memorial Women's Hospital in Nagpur has screened around 10,000 pregnant women annually and treats almost 1,500 sickle-cell patients each year. Through CSR partnerships, they provide financial aid up to ₹12 lakh for transplants.
International Steps in India
- British researcher Lucy Wills' early work in Bombay had a global impact. Her folate discovery revolutionized prenatal care worldwide. Today, her legacy continues with folic acid supplementation as part of maternal health protocols.
- Global recognition and collaboration with ICMR, WHO, and UNICEF supported India's Anemia Mukt Bharat strategy, which integrates international guidelines on supplementation, food fortification, and behavioural change.
Rural and Citizen-Led Initiatives
- In states like Haryana, local doctors report seeing over 50% of patients anaemic, mainly women. Social media threads highlight that vegetarian diets, tea intake, and boiled vegetables lacking vitamin C contribute to poor iron absorption.
- The concept of "Tithi Bhojan" in Gujarat and other states involves local communities donating nutritious meals to government school midday meals, supporting iron-rich dietary intake among children.
- In tribal zones like Gumla, besides screening, villagers participate in Anganwadi programs, community mobilization for nutrition kits, and awareness events, displaying grassroots ownership of Anemia prevention.
Awards & Recognition
- Prof. J.B. Chatterjea (Kolkata) received prestigious honors, including the Shanti Swarup Bhatnagar Prize (1966), Asiatic Society Barclay Medal (1963), and ICMR Basanti Devi Prize (1964), for his hematology research on thalassemia and blood disorders.
- Dr. Yazdi Maneksha Italia was awarded the Padma Shri in Medicine (2024). His leadership in tribal sickle-cell control also earned the PM's Award for Excellence and Health Leader of the Year status.
Past and Present Statistics on Anemia in India
Anemia is one of India's most persistent public health problems. It affects millions of women, children, and adolescents-and despite decades of effort, the rates are still alarmingly high.
A. NFHS-4 (2015-16): The Starting Point
The National Family Health Survey - 4 (NFHS-4) painted a bleak picture:
- Children (6-59 months): 58.6% were anaemic
- Women (15-49 years): 53.1%
- Pregnant women (15-49 years): 50.4%
- Adolescent girls (15-19 years): 54.1%
The situation was particularly bad in rural and low-income groups, where access to iron-rich diets and healthcare was limited.
B. NFHS-5 (2019-21): The Setback
The National Family Health Survey - 5 (NFHS-5) showed that things had worsened:
- Children (6-59 months): 67.1% (↑ from 58.6%)
- Women (15-49 years): 57.0% (↑ from 53.1%)
- Pregnant women: 52.2% (↑ from 50.4%)
- Adolescent girls: 59.1% (↑ from 54.1%)
Instead of improving, Anemia prevalence rose in nearly every group. Even states with better healthcare, like Kerala and Tamil Nadu, saw a rise. States like Gujarat, Bihar, and Madhya Pradesh remained among the worst-affected.
C. Why the Increase?
Health experts believe multiple factors are at play:
- Poor absorption of iron due to chronic infections or gut issues
- Gaps in IFA supplement supply or compliance
- Lack of dietary diversity
- Overreliance on pill-based interventions without fixing root causes
- Inadequate food fortification in public systems
D. Where We Stand Now (2023-24)
We're still waiting on NFHS-6, which may show the post-pandemic impact. But preliminary data from the Health Management Information System (HMIS) still show that more than half of pregnant women and adolescent girls have low haemoglobin.
Anemia is also one of the top contributors to Years Lived with Disability (YLDs) for Indian females aged 10-49.
Despite large-scale schemes like Anemia Mukt Bharat and POSHAN Abhiyaan, the real impact on the ground is mixed.
Conclusion
Anemia is preventable and treatable. But we need more than medicine to beat it. It requires changes in diet, strong communities, and consistent health policies. India's government has rolled out smart schemes, but the real test lies in reaching the hardest-to-reach. This will take years of commitment: raising awareness, improving nutrition, and building a responsive health infrastructure, and the Indian Government is continuously working towards it. And that's how Anemia can finally stop getting in the way of India's future.
References
- NFHS‑5: Anemia among women, children, men
- Increase in child Anemia NFHS‑4 to NFHS‑5
- Overview of AMB strategy
- IFA distribution Q2 FY 2024‑25
- Anemia prevalence spikes
- Lucy Wills discovery (folate and macrocytic Anemia, Bombay): https://en.wikipedia.org/wiki/Lucy_Wills
- https://embryo.asu.edu/pages/treatment-anemia-during-pregnancy-1931-lucy-wills
- Dr. Yazdi Maneksha Italia was awarded Padma Shri for his work in Gujarat: https://www.devdiscourse.com/article/headlines/2904819-recognition-of-my-work-has-been-given-padma-shri-award-yazdi-maneksha-italia
- Sickle cell awareness in Odisha and Chhattisgarh: https://timesofindia.indiatimes.com/city/bhubaneswar/tribals-screened-for-sickle-cell-disease/articleshow/97753206.cms
- Gumla's 100% sickle screening and welfare camps: https://timesofindia.indiatimes.com/city/ranchi/special-camps-in-gumla-links-hundreds-with-welfare-schemes/articleshow/122347749.cms
- Controversial UK radiological study (radioactive chapatis, Coventry 1969): https://time.com/5587196/lucy-wills-google-doodle/