Introduction to COVID-19 in India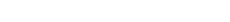
COVID-19, short for Coronavirus Disease 2019, first begins in Wuhan, China, in late 2019. Since then, it has evolved into the fifth recorded pandemic in modern history, following the 1918 flu pandemic. By September 2021, the global toll included over 200 million confirmed cases and more than 4.6 million lives lost.
India, with over 1.4 billion people, faced a complex battle. The virus spread quickly through both urban slums and rural villages. Hospitals were overwhelmed, lockdowns halted economies, and millions faced food and job insecurity. Schools closed, exposing the digital divide in education. The crisis exposed deep gaps but also sparked resilience, innovation, and a nationwide push toward better preparedness.

Dec 2019
First identified (Wuhan)
Respiratory
Primary system affected
Vaccines
Mass rollout from Jan 2021
Variants
Delta, Omicron & subvariants
Introduction to COVID-19
COVID-19, caused by the SARS-CoV-2 virus, first appeared in Wuhan, China, in December 2019. Initially seen as a local health issue, it rapidly escalated into a global pandemic, disrupting nearly every aspect of modern life. The virus, mainly spread through respiratory droplets, moved across borders at an alarming speed. The World Health Organization declared it a global health emergency within weeks, and countries worldwide scrambled to respond.
India, with over 1.4 billion people, faced a complex battle. The virus spread quickly through both urban slums and rural villages. Hospitals were overwhelmed, lockdowns halted economies, and millions faced food and job insecurity. Schools closed, exposing the digital divide in education. New variants kept emerging, forcing constant updates in health protocols. Despite all odds, India ramped up vaccine production, scaled testing, and mobilized health workers nationwide. The crisis exposed deep gaps but also sparked resilience, innovation, and a nationwide push toward better preparedness.

Why it mattered
The pandemic exposed gaps in healthcare, social protection and supply chains, while demonstrating the power of coordinated public health action, vaccine development, and community mobilisation.
What Is COVID-19?
COVID-19 is an infectious disease caused by a novel strain of coronavirus known as SARS-CoV-2. This virus belongs to a larger family of coronaviruses, some of which are known to cause illnesses ranging from the common cold to more severe diseases such as SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome). SARS-CoV-2 was first identified in December 2019 and has since caused one of the most widespread pandemics in recorded history.
The virus primarily targets the human respiratory system. Once inside the body, it attaches to receptors in the lungs and airways, leading to a range of symptoms. While many individuals experience mild to moderate symptoms such as fever, cough, and fatigue, others develop serious complications, including pneumonia, acute respiratory distress syndrome (ARDS), and in some cases, multi-organ failure. People with existing health conditions, the elderly, and those with weakened immune systems are at higher risk of severe illness.
As the virus circulated globally, it began to mutate. Several variants of concern have emerged, including Delta and Omicron. These variants differ in transmissibility, severity, and their response to vaccines or prior infection. Monitoring and responding to these changes remain essential for ongoing disease control.
How COVID-19 Spreads
COVID-19 spreads mainly through respiratory droplets when an infected person coughs, sneezes, talks, or breathes. In closed or poorly ventilated spaces, the virus can linger in the air as tiny particles, raising the risk of airborne spread. It can also pass through contact with contaminated surfaces like phones, railings, or doorknobs, followed by touching the face. Crowded events like weddings, rallies, or religious gatherings often become super-spreader hotspots. Even people without symptoms can unknowingly transmit the virus, making it harder to control. Simple steps like wearing masks, keeping distance, and improving airflow are vital to slowing transmission and keeping communities safer.
High-risk settings
- Closed, crowded, and poorly ventilated indoor spaces
- Mass gatherings, religious events, and crowded transport
- Healthcare settings without proper PPE
Who Is Most at Risk?
COVID-19 can affect anyone, but certain groups are more vulnerable to severe illness and complications. Age, existing health conditions, and exposure levels play a major role in determining risk.
The most at-risk populations include:
- Adults over the age of 60
- Individuals with chronic illnesses such as diabetes, hypertension, or heart disease
- People with asthma or other respiratory conditions
- Cancer patients and transplant recipients with suppressed immunity
- Frontline workers in healthcare, sanitation, and essential services
- Individuals living in overcrowded or underserved communities
- Unvaccinated persons and those with compromised immune systems
Timely protection, regular monitoring, and early intervention remain critical for these groups.
Symptoms of COVID-19
COVID-19 symptoms vary widely in severity and duration. While many people develop mild symptoms, others may experience serious complications requiring hospitalisation.
Common symptoms
- Fever or chills
- Dry or persistent cough
- Sore throat
- Fatigue or general weakness
- Loss of taste or smell
- Headache or body aches
These signs often resemble seasonal flu, making early detection important.
Severe symptoms (seek urgent care)
- Shortness of breath or laboured breathing
- Chest pain or tightness
- Oxygen saturation dropping below 94%
- Confusion, difficulty waking, or extreme drowsiness
Long COVID symptoms (lasting weeks or months):
Some people experience persistent symptoms for weeks or months, including:
- Constant fatigue despite rest
- Brain fog or poor concentration
- Muscle or joint pain
- Breathlessness during light activity
Not everyone experiences all symptoms, and some cases remain asymptomatic. People with mild illness should still isolate and monitor their condition closely. For those in high-risk categories, any sign of worsening symptoms should prompt urgent medical evaluation.
When to test
Test if symptomatic, after exposure to a confirmed case, or before high-risk visits (elderly, hospital). Use RAT for quick screening and RT-PCR for confirmation.
Diagnosis and Testing
Accurate and timely diagnosis plays a critical role in controlling the spread of COVID-19. Multiple testing methods have been deployed across India to identify active cases, trace contacts, and guide treatment decisions.
- The RT-PCR (Reverse Transcription Polymerase Chain Reaction) test is considered the gold standard for COVID-19 detection. It identifies the genetic material of the virus and is highly accurate, especially in the early stages of infection.
- Rapid Antigen Tests (RATs) provide quicker results, usually within 15-30 minutes. However, they are less sensitive and may miss some positive cases, especially if the viral load is low.
- Antibody tests detect the presence of antibodies in the blood, indicating past exposure to the virus. These are not used to diagnose active infections but help in understanding population-level immunity.
- Home testing kits, approved by regulatory bodies, allow individuals to self-test with proper instructions. These kits offer convenience and reduce testing burden at centres, though results must still be reported for official tracking.
Variants and Waves in India
India has witnessed multiple COVID-19 waves, each shaped by different variants and evolving public response.
The first wave in 2020 saw a gradual spread of infections, largely contained through an early nationwide lockdown. Though movement was restricted, health systems were able to manage cases during this phase.
The second wave in 2021 was driven by the Delta variant, leading to a national health crisis. The shortage of oxygen and a sharp rise in deaths overwhelmed hospitals across the country. This wave exposed critical gaps in infrastructure and prompted emergency interventions.
In early 2022, the third wave was dominated by the Omicron variant, which spread rapidly but caused milder symptoms in most people. Although cases surged, the rate of hospitalisation remained lower due to prior immunity and vaccine coverage.
India's INSACOG (Indian SARS-CoV-2 Genomics Consortium) monitors variants through genomic sequencing to guide public health response.

Treatment and Remedies for COVID-19
Treatment for COVID-19 depends on the severity of symptoms and individual health conditions. India has followed a tiered approach to manage cases, ranging from home isolation to intensive hospital care.
A. Home-Based Management
Most mild or asymptomatic cases can be safely managed at home under proper guidance.
- Patients must remain isolated to prevent transmission within households.
- Hydration and adequate rest support the body's natural recovery process.
- Paracetamol is commonly used to reduce fever and relieve body aches.
- Pulse oximeters help monitor blood oxygen levels, especially when fatigue or breathlessness is present. A drop below 94% requires medical attention.
- Supportive measures such as steam inhalation and saline gargles may relieve throat irritation and congestion.
- Clear instructions from healthcare professionals, along with regular check-ins, are essential during home recovery.
B. Hospital Care
Moderate to severe cases need hospitalisation and specialised treatment.
- Oxygen therapy is provided when blood oxygen levels fall. This may range from nasal oxygen to high-flow support.
- Antiviral drugs like remdesivir may be used in select cases with early symptoms, though their benefits are limited.
- Steroids such as dexamethasone are administered to reduce inflammation in severe cases.
- Monoclonal antibodies are considered for high-risk patients in early stages to prevent disease progression.
- In critical cases, ventilatory support, including non-invasive ventilation (NIV) or mechanical intubation, may be required.
- Convalescent plasma therapy, once explored as a treatment, is now discouraged due to insufficient evidence of effectiveness (ICMR Advisory).
- Protocols are regularly updated based on national and international clinical data.
C. Recovery and Post-COVID Care
Recovery does not end with a negative test. Many patients, especially those with moderate to severe illness, require ongoing support.
- Breathing exercises and chest physiotherapy help restore lung function.
- Nutritional care is important to rebuild strength and immunity.
- Follow-up consultations ensure complications such as lung fibrosis or cardiac issues are detected early.
- Many patients benefit from mental health counselling, especially after long hospital stays or ICU admissions.
- Those with Long COVID symptoms like fatigue, brain fog, or joint pain may need structured rehabilitation programs for full recovery.
India's public health system continues to support COVID-19 care through evolving clinical guidelines and community-based rehabilitation.
Quick checklist
- ✓ Isolate if positive
- ✓ Monitor oxygen levels
- ✓ Stay hydrated and rest
- ✓ Seek urgent care for red flags
Vaccination in India
India's COVID-19 vaccination programme has been one of the largest in the world, both in scale and speed. Multiple vaccines have been developed or approved for emergency use within the country.
A. India's Vaccines
- Covaxin, developed by Bharat Biotech, is an inactivated virus-based vaccine.
- Covishield, produced by the Serum Institute of India in collaboration with Oxford-AstraZeneca, is a viral vector vaccine.
- Corbevax, developed by Biological E, is a protein subunit vaccine approved for children and adults.
- Other vaccines like Sputnik V, ZyCoV-D, and Covovax were also introduced as part of the national vaccination effort.
B. Phased Rollout
India adopted a phased rollout approach, starting in January 2021.
- Frontline workers and healthcare personnel were prioritised.
- This was followed by the elderly and those with comorbidities.
- The programme then expanded to the entire adult population, and later to children.
- The CoWIN portal was used for registration, slot booking, and digital certification.
- In rural and hard-to-reach areas, walk-in registrations and door-to-door campaigns ensured broader access.
C. Impact of Vaccination
- Vaccines played a crucial role in reducing hospitalisation and mortality, especially during later waves.
- Though breakthrough infections occurred, they were generally mild in vaccinated individuals.
- A booster dose, or precautionary dose, was introduced to maintain immunity over time.
- Addressing vaccine hesitancy became a major focus, with government and community-led awareness campaigns across states.
- The vaccination drive continues to evolve with emerging data and newer variants.
Fatality and Long-Term Impact
India officially reported over 5 lakh COVID-19 deaths, but many experts believe the real toll is higher due to underreporting, especially in rural areas and home deaths. The loss of primary earners devastated families, leaving many orphans and elderly dependents. Mental health struggles like anxiety, depression, and trauma surged across age groups. Long COVID symptoms, including fatigue, breathlessness, and brain fog, continue to disrupt lives and affect productivity.
Children faced major setbacks with schools shut for months, impacting learning, social growth, and emotional well-being. Many households slipped into financial distress due to job losses and healthcare costs. The pandemic's lasting effects go beyond infection numbers. It exposed gaps in public health, disrupted livelihoods, and stressed the need for stronger support systems moving forward.
Government Schemes and Support for COVID-19 in India
The Government of India adopted a multi‑faceted response to the COVID‑19 pandemic, combining stringent containment measures, healthcare system strengthening, financial support, and digital innovations.
A. Emergency Response
- In March 2020, a nationwide lockdown was implemented to slow viral transmission, restricting mobility and public gatherings while maintaining essential services.
- Containment zones were declared in high-infection areas, supported by surveillance and active case finding.
- Clear protocols for home and institutional quarantine and isolation were issued via the Ministry of Health and Family Welfare.
- The Aarogya Setu app was launched nationally to facilitate contact tracing, risk alerts, and self-assessment tools.
B. Health Infrastructure Boost
- Thousands of temporary COVID Care Centres were set up in public spaces such as stadiums and schools.
- Public hospitals scaled up ICU beds and established oxygen generation plants to meet demand.
- PPE kits, ventilators, and other medical supplies were distributed across states.
- Free RT‑PCR testing became available in public facilities, while the number of testing labs across districts grew significantly.
C. Policy and Finance
- The PM CARES Fund, set up on March 27, 2020, serves as a public charitable trust to support healthcare infrastructure, vaccine research, and direct relief during the health crisis. The fund is chaired by the Prime Minister with key ministers as trustees; it accepts only voluntary donations and does not receive budgetary allocations.
- Central authorities allocated oxygen, ventilators, and critical supplies to states based on caseload and need.
- Regulatory limits were imposed on testing charges, hospital fees, and oxygen cylinder prices to prevent profiteering.
- The Pradhan Mantri Garib Kalyan Package included insurance cover and compensation for frontline workers who died in service.
- Vaccines were procured in bulk centrally and distributed free to all adults under government programmes.
D. Digital Tools
- CoWIN, the central vaccination management platform, handled registration, slot booking, dose scheduling, and certificate issuance.
- Aarogya Setu continued to support the detection of exposure risk and awareness messaging.
- The e‑Sanjeevani telemedicine portal, India's national telehealth service, enabled free online consultations, especially vital during lockdowns and for rural populations. It is estimated to have served crores of users and continues operating across thousands of centres.
This integrated strategy, comprising containment, infrastructure enhancement, policy support, and digital innovation, formed the backbone of India's pandemic response.
Key Schemes and Relief Measures
During the COVID‑19 crisis, the Government of India rolled out relief measures targeting healthcare, nutrition, livelihood, and social security.
- A nationwide free vaccination drive covered all adults (18+) under the central immunisation programme via CoWIN.
- The Pradhan Mantri Garib Kalyan Package (PMGKP), announced on 26 March 2020 and valued at ₹1.70 lakh crore, included: Insurance cover of ₹50 lakh per health worker involved in COVID‑19 care, reaching around 22 lakh workers.
- Distribution of free foodgrains: 5 kg wheat or rice per person plus 1 kg pulses per family to about 80 crore poor beneficiaries under PMGKAY.
- The Pradhan Mantri Garib Kalyan Anna Yojana (PM‑GKAY) food subsidy scheme was extended through multiple phases, distributing over 111.8 lakh metric tonnes of food grains to ~80 crore beneficiaries until late 2022 and beyond.
- The Emergency Credit Line Guarantee Scheme (ECLGS) provided urgently needed credit support for MSMEs to preserve livelihoods during the lockdown.
- Under Ayushman Bharat - PMJAY, eligible individuals received free COVID‑19 hospitalisation at empanelled facilities.
- eSanjeevani, the national telemedicine platform, enabled millions to access free online consultations from home or primary centres. Over 3 crore teleconsultations were delivered, and today it operates at scale in 31 states/UTs across Ayushman Bharat Health & Wellness Centres.
- Mental health helplines and counselling portals were activated nationwide to support those dealing with stress, grief, or anxiety.
These schemes formed the cornerstone of India's pandemic response, helping millions stay safe, fed, and financially supported during an unprecedented emergency.

Key Steps in Medical Science in India
India's scientific achievements during COVID‑19 were historic:
- Through Mission COVID Suraksha under the Department of Biotechnology, India funded and fast‑tracked four indigenous vaccines like ZyCoV‑D, Corbevax, GEMCOVAC‑19, and iNCOVACC, cutting timelines dramatically.
- Regulatory acceleration by CDSCO enabled the rapid approval of vaccines, diagnostics, and therapeutics.
- India emerged as a vaccine superpower, manufacturing nearly 60 percent of the global vaccine supply, with leadership by institutions like ICMR, Bharat Biotech, and Serum Institute.
- The WHO's emergency use listing of Covaxin in November 2021 gave global recognition to India's vaccine programme.
These steps reflect India's collaborative efforts across science, industry, and governance to deliver affordable vaccines at scale.
Major Steps in States of Gujarat, Bihar & Jharkhand
Gujarat
- After its first cases in March 2020, Gujarat adopted a testing‑tracking‑treatment approach rather than a full lockdown.
- Testing increased from around 64,000 in April to nearly 3,91,000 by July, about three times the ICMR recommended rate.
- Received positive recognition from WHO for initiatives like Dhanvantari Rath, fever helplines, and Sanjivani Vans.
- Regional voluntary curfews enforced via local markets and associations instead of formal lockdowns.
- Use of mobile apps like Dr TeCHO and home quarantine tracking systems for surveillance and reporting.
Bihar
- The state used a custom app, Garuda, to register and monitor incoming international travellers.
- Field teams conducted daily health checks and data entry via the SEOC/DEOC system.
- Support to migrants included the Aapda Sampoorti Portal, which offered ₹1,000 direct transfer to stranded labourers.
- The Garib Kalyan Rojgar Abhiyaan, rolled out in June 2020 across 32 districts, provided work and rural infrastructure development for returnee migrants.
Jharkhand
- Jharkhand maintained alertness into 2025, issuing circulars after detecting new infections in May.
- Healthcare preparedness included activating isolation wards, ventilators, and 150 ICU beds at RIMS, Ranchi.
- A virology centre at Sadar Hospital, Ranchi, is set to begin RT‑PCR testing to reduce load on RIMS.
- Digital education continuity was ensured via Project Gyanodaya, which broadcast online classes on DD Jharkhand and distributed tablets to students.
Major News Highlights and Awards for COVID-19
News Highlights for COVID
A few key national and state developments featured prominently in the media:
- Earlier this year, a CAG report found Andhra Pradesh spent ₹4,606 crore on COVID‑19 management between 2019-20 and 2022-23. Rapid expansion of testing labs (135) and treatment centres (260→640 hospitals), and full vaccination coverage are notable achievements.
- Reports noted a recent mild resurgence of infections in states like Maharashtra and Andhra Pradesh, tied to emerging Omicron subvariants such as OF.7 and NB.1.8. Experts pointed to waning immunity and renewed emphasis on booster campaigns.
- The Centre recently announced an increase in monthly incentives for ASHAs from ₹2,000 to ₹3,500, alongside higher retirement benefits (₹50,000), addressing long-standing demands from frontline health workers.
International Steps in India
- The WHO's emergency-use approval of Covaxin in November 2021 allowed India to supply vaccines to low‑income countries through COVAX, enhancing global equity.
- India exported vaccines to over 100 countries while scaling domestic coverage to nearly 1.56 billion doses and fully vaccinating 77% of adults within a year.
- The Serum Institute of India, working with AstraZeneca, played a pivotal role in global supply, producing vaccines affordably at scale. They further developed pandemic preparedness capacity for future outbreaks.
- Indian institutions also supported the WHO and G20 health initiatives, emphasizing equitable access to countermeasures. India's leadership was officially acknowledged by WHO chief scientist Jeremy Farrar.
Rural Initiatives & Citizen Actions
- In Andhra Pradesh, the government conducted house visits to over 1.4 crore rural households, distributing masks and identifying symptomatic individuals for testing.
- Kerala's Kudumbashree mission, largely driven by women self-help groups, set up community kitchens, produced masks and sanitizers locally, managed elderly care, and offered psychosocial support.
- Rural citizens organized grassroots awareness drives, mobilized farmers' collectives, and educated communities about isolation, hand hygiene, and social distancing. Village panchayats used public address systems and local networks to reinforce COVID protocols.
Award / Rewards
- The Kayakalp Award, conferred by the Ministry of Health and Family Welfare, recognised excellence in infection control and hygiene in public health centres during the pandemic. Many COVID‑care facilities across states earned this honour.
- Dr Pragya D. Yadav, a lead NIV virologist, received numerous honours, including the COVID Warrior Award (Governor of Maharashtra, 2020), Dr Pran Nath Chhuttani Oration, and others from ICMR and National Academy of Medical Sciences.
- State awards like Champions of Change acknowledged civil and health leaders in Maharashtra and Telangana involved in the COVID response and public service.
Past and Present Statistics on COVID-19 in India
COVID-19 reshaped public health in India almost overnight. What started as a single case in early 2020 grew into a nationwide crisis. The numbers, responses, and aftershocks have defined healthcare, politics, and the economy for years.
A. The First Wave (March-Dec 2020): The Beginning
- India's first case was reported on January 30, 2020, in Kerala.
- A national lockdown began on March 24, 2020, bringing life to a halt.
- By December 2020:
- 10.3 million confirmed cases
- 1.5 lakh deaths
- Urban areas like Mumbai, Delhi, and Chennai were hardest hit.
- Testing and hospital capacity were limited in the early months.
- Migrant workers' crisis exposed cracks in urban planning and healthcare support.
B. The Second Wave (March-June 2021): The Deadliest Phase
This wave hit fast and hard, driven by the Delta variant.
- Daily cases peaked at over 4 lakh in May 2021.
- Hospitals collapsed, oxygen shortages, no ICU beds, and mass cremations dominated headlines.
- Official death toll: Over 4 lakh, but estimates suggest the real number may have been 3 to 4 times higher.
- Rural India was deeply affected, with minimal testing or care access.
The wave exposed how underprepared India was for a pandemic of this scale.
C. Vaccination and Recovery (Late 2021-Early 2022)
- India rolled out its vaccine program on January 16, 2021.
- Covishield and Covaxin were the primary vaccines.
- By January 2022:
- Over 1.5 billion doses administered
- Focus on adult population, then 15-18 age group
- Vaccination helped reduce hospitalisation and deaths in future waves.
The government also launched CoWIN, a digital platform for vaccine booking and tracking, which became a model for other countries.
D. The Omicron Wave (Dec 2021-Feb 2022)
Omicron triggered a huge rise in cases, but with fewer deaths.
- Daily cases crossed 3 lakh, but hospitalisation remained low.
- Reinfections became common, but most cases were mild.
- Vaccine boosters were introduced for frontline workers and seniors.
E. Current Picture (2023-24)
- As of mid-2024, India had recorded over 45 million confirmed cases and more than 5.3 lakh official deaths.
- Seroprevalence surveys suggest that over 90% of Indians have antibodies from infection or vaccination.
- COVID is now managed like any other respiratory illness in most hospitals.
- Vaccination coverage is over 90% in adults for the primary dose; booster uptake is lower.
- Localised outbreaks still occur, especially with new variants, but are mostly under control.
F. Why COVID's Impact Was So Deep
- Population density and mobility made rapid spread unavoidable.
- Gaps in rural healthcare delayed diagnosis and care.
- Misinformation and vaccine hesitancy slowed response.
- Economic shocks from lockdowns hurt millions, especially in the informal sector.
What's Next?
COVID may never fully disappear. But with immunity, vaccine access, and better systems in place, India is better prepared.
Future plans include:
- Better disease surveillance through platforms like IDSP and CoWIN+
- Stockpiling of critical resources like oxygen, PPE, and essential medicines
- Strengthening primary healthcare and digital health records
Conclusion
COVID-19 changed the way India and the world thought about public health. It exposed deep gaps in our systems but also showed what's possible when science, policy, and people align. From mass vaccination to grassroots awareness campaigns, the country saw both pain and progress. Yes, mistakes were made. But millions of lives were saved, too. Now is the time to learn, not forget. To invest, not ignore. A stronger, more resilient healthcare system won't build itself. It needs effort from every level of government, community, and each of us. Because health is not a luxury. It's a shared responsibility.
Key Takeaways
- COVID-19 was unprecedented in scale and impact
- Vaccination saved millions of lives
- Digital health infrastructure proved critical
- Community involvement was essential
- Preparedness is key for future pandemics
Moving Forward
- Strengthen primary healthcare systems
- Invest in disease surveillance
- Maintain vaccine infrastructure
- Support mental health services
- Build community resilience
References and Resources
Indian Government Resources
- Ministry of Health and Family Welfare, Government of India.
https://www.mohfw.gov.in - Indian Council of Medical Research (ICMR) COVID-19 Updates.
https://www.icmr.gov.in - CoWIN Vaccination Portal, Government of India.
https://www.cowin.gov.in - Press Information Bureau - COVID-19 Bulletins.
https://pib.gov.in/PressReleasePage.aspx - National Health Authority - Ayushman Bharat Updates.
https://nha.gov.in
International Health Organizations
- World Health Organization - India COVID-19 Dashboard.
https://www.who.int/india - UNICEF India - COVID-19 and Children's Health.
https://www.unicef.org/india/coronavirus
Media and Research
- Economic Times - India's Oxygen Crisis Explained.
https://economictimes.indiatimes.com/news/india/indias-oxygen-crisis-explained - Times of India - COVID-19 Vaccination Drive Progress.
https://timesofindia.indiatimes.com/india - The Hindu - Challenges in Rural COVID-19 Management.
https://www.thehindu.com/news/national/covid-in-rural-india - IndiaSpend - COVID-19 Data Tracking and Analysis.
https://www.indiaspend.com - The Lancet - India's COVID-19 Surge and Public Health Lessons.
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)01275-2/fulltext
Stay Safe — Vaccinate and Test
Get vaccinated, test if symptomatic or exposed, and follow public health guidance to protect yourself and others.